Last week, Mark (the hubby) asked his bachelor colleague on breastfeeding advice – this week, Kate asks her BFF. What will happen with these 2 VERY DIFFERENT advice? From friends who are single?! Follow this breastfeeding cartoon series here.
So, is drinking 8 glasses of water good for skin?
There is little research to back up that drinking more water is going to hydrate the skin, make the skin glow or smooth. The practical reason for this is that research is usually conducted for ‘products’ when they can be patented, thus the lack of research on water. The only research that I can find on Pubmed on water is Effect of fluid intake on skin physiology: distinct differences between drinking mineral water and tap water. The results seemed convoluted though with no clear conclusion.
The conclusion from most dermatologists though is lack of water is bad for the skin but excess water does not benefit the skin.
What happens to Skin when Drinking Too Little Water?
Our body needs water for its organs to function so it will reduce hydrating cells to channel water for essential body functions. The skin will then look duller and wrinkles and pores will be more apparent. However, there is no change to the underlying skin structure but the wrinkles and pores are ‘temporarily’ more obvious when the body is dehydrated. But prolonged dehydration can speed up aging as the skin is persistently drier and more prone to skin irritation as well.
So, does Drinking Water Help with Hydrating Skin?
Water that we drink does not go straight to the skin – it goes to intestines, bloodstream, filtered by kidneys. If you drink excess water, the body will pass it out – it wouldn’t go specifically to hydrating skin cells although water will hydrate all cells in general. To target skin cells, moisturizing is required and avoid doing a list of things that will actually dry your skin such as:
1. Scrubbing or exfoliating your skin
2. Drying (instead of dabbing dry) with a towel
3. Sun-tanning (and not using sunscreen)
4. Long bath and Hot bath
5. Using soap
6. Not eating enough omega 3 (which our diet is generally lacking in, essential fatty acids)
Bottom line – Drink when you’re thirsty.
Signing off SkinishMom, and yes, just remembered that thirst is often mistaken for hunger so I’m drinking up!
Eczema ‘Cure’ Series – Home Remedies
If you’ve been following this blog, you’d know I don’t jump into eczema (miracle) cures. I still don’t.
But as I read journeys of how eczema sufferers are cured, I realized that there are common approaches they take. These may not be THE (or even an) eczema cure but I think there’re certain situations which they may help improve eczema. I hazard a guess and this series is more about a holistic approach to controlling eczema – I suppose you can call it a cure if one approach singularly works well for you!
Many eczema sufferers are wary of chemical and steroids. I agree but am also wary of going into extremes of attributing everything bad to chemicals and steroids, especially given that eczema is a condition that comes about from many factors (so would focusing on just one aspect be over-simplification?). But I’m definitely supportive of home remedies that work – if they work without side effect!
Home Remedy #1 – Moisturize
Moisturizing is one approach that most would agree is beneficial. It’s accepted that eczema patients (adults and children) have defective skin barrier and a moisturizer have various functions to
- Protect skin from drying/ losing too much moisture
- Protecting skin from irritants
- Absorbing water into the skin
- Filling up the ‘holes’ in the skin or restoring the skin lipids (that help keep the skin cells together and prevent infection, learn more from dermatologist Dr Cheryl Lee in this Over-Alkaline skincare interview)
See also the research on moisturizing where it had been shown to reduce steroid usage and preventive effect on babies with high risk
Watch the video on how to moisturize baby’s sensitive skin.
Home Remedy #2 – Don’t Moisturize (with Irritants)
There are also sharing by eczema sufferers that their eczema improved after STOPPING moisturizer use. My guess is that there could be ingredients in the moisturizers that they have been using that are triggering the eczema, a form of contact dermatitis. There is a test to determine which ingredient in skincare product that you could be sensitive to, known as patch test (interview with Laura Verallo Rowell, CEO of VMV Hypoallergenics).
There are indeed individuals whose skin are sensitive to many common ingredients and therefore, it would make sense for this selected group to stop moisturizer use. Not for general population with dry skin though.
To be safe, start off with a moisturizer that doesn’t contain the top irritants, compiled by dermatologist Dr Verallo Rowell with alternative names to these irritants.
Home Remedy #3 – Keep the Skin Moist
I wouldn’t really call it a ‘home remedy’ as clothing products that are able to trap moisture close to the skin and studied to improve eczema usually have invested money into the technology behind the clothing. One such technique is Wet Wrap which had been shown to help eczema and if you’d like to know more about what goes into the wrap and how to use it, read here. My national (Singapore) eczema support group also runs regular wet wrap session, do sign up at the top right box of my blog to be kept posted!
Home Remedy #4 – Ways to Kill Staph Bacteria
Staph bacteria is a common cause for eczema where increasing research showed that eczema skin is colonized by this bacteria which produces toxins that can worsen skin inflammation. There are ‘natural’ ways to kill the bacteria, for instance swimming or bleach bath or shower with a chlorhexidine-based bath wash.
If you don’t like the idea of bleach, read this interview with dermatologist Dr Cheryl Lee on vinegar spray.
Home Remedy #5 – Oils
Though no conclusive research, there are eczema patients whose skin improved after primrose and borage oil (see dermatologist Dr Cynthia Bailey’s comment in the post) and virgin coconut oil (see this very informative interview with dermatologist Dr Verallo Rowell on different types of coconut oil – make sure you get the right type!)
Home Remedy #6 – Anti-Inflammatory Natural Ingredients
There are also quite a few natural ingredients that have anti-inflammatory properties like honey, lavendar or able to protect skin like colloidal oat (interview with dermatologist Dr Claudia Aguirre).
Personally, I feel that the biggest home remedy is to avoid triggers. Logically it makes sense to identify these triggers because no treatment or remedy can be helpful if the skin is under constant ‘attack’. After which, I do believe in moisturizing and as for using natural ingredients, I’m all for it as long as it’s not something that irritate you (beware that natural does not equal no hypersensitive reaction) nor past expiry (as a home-made product may be less stable so the expiry date matters more).
Mark is consulting his colleague for breastfeeding advice… Wrong move. Follow this breastfeeding cartoon series here.
MarcieMom was interviewed on her daily life with Marcie here (for a fellow mom’s business whose daughter Patricia also had eczema). Thought it’d be good to share with everyone her routine and the ‘quirks’ of taking care of an eczema child.
Morning
I wake up around 7am and get Marcie ready for the school bus. Our mornings in the week always involve applying lots of moisturiser and sometimes it can be a struggle but the afternoon on weekdays are my breather because I work while Marcie is in preschool.

Afternoon
At the weekend, our afternoons are for finishing up homework and then going for a quick shower to freshen up and clean off sweat residue to help Marcie cool down in the hot Singapore weather, followed by moisturising with an intensive cream. We always use a thicker cream in the afternoon as the next time we moisturise Marcie will be bedtime, which can be quite a few hours away!
Evening
When it comes to the weekend evening, we take her swimming to kill the staph bacteria. When her eczema is itchy we use lots of different techniques to distract and keep her happy which I wrote about in this post. My favourite is always letting her play with ice. This is because it’s free of charge – and easy to wipe up! Now that Marcie is older, she doesn’t play with ice as much but we always order ice water for her still.

One advice
My advice to other parents who have a child who suffers with Eczema, is to stick with your spouse as both of you will be pillars of support for each other and to have faith. Also, take time to relax and never blame yourself.
What is your day like? Share in the comments!
Eczema ‘Cure’ Series – Diet
If you’ve been following this blog, you’d know I don’t jump into eczema (miracle) cures. I still don’t.
But as I read journeys of how eczema sufferers are cured, I realized that there are common approaches they take. These may not be THE (or even an) eczema cure but I think there’re certain situations which they may help improve eczema. I hazard a guess and this series is more about a holistic approach to controlling eczema – I suppose you can call it a cure if one approach singularly works well for you!
Now, many eczema sufferers report curing their eczema from eliminating certain foods from their diet, typically these are (i) diary, (ii) wheat and (iii) sugar. Is there a basis for this? Think along with me!
Suspect #1 – Allergy to Diary and Wheat Undetected
This is the most straightforward reason why cutting certain foods from diet heal your eczema – it’s possible that you have an allergy to certain foods but you’re not aware of it. The unawareness could be due to:
- You have not taken an allergy test, be it either skin prick test or blood IgE test. Watch the video on allergy testing and #SkinishMom column on why sometimes doctors don’t get you tested (other than the other obvious reason which is they don’t have the facility to test and don’t want to refer you to another doctor..)
- Foods like diary and wheat are so prevalent in our diet that you may not notice. Generally speaking the more common something is, the less likely that you can identify it on your own as the trigger for your eczema. That is why although house dust mite is a very common trigger, parents tend to not associate their child’s eczema flare up with it. For common allergens for children of different age, see here (extracted from Professor Hugo Van Bever’s article – Prof Hugo is my co-author for Living with Eczema Mom Asks, Doc Answers!)
Suspect #2 – Food Intolerance or Hypersensitivity not Easily Tested
While allergy testing (for increased blood IgE immunoglobulin) is straight forward, detecting food intolerance or hypersensitivity is a whole different ball game. Even allergist or your nutritionist can be floored by it. For instance, reaction to a food intolerance can be gradual, not necessarily in small amount (unlike allergy) and can be intolerant only when certain foods are in certain state (eg raw versus cooked). Learn more on the differences between allergy and food intolerance.
As such, it could well be that your intolerance reaction is in the form of skin rash but because it is delayed reaction, no doctor has told you that a certain food is the culprit. However, when it is removed from your diet, your skin condition improves.
Here’s an interesting research on how children have tummy ache but didn’t get diagnosed as related to food sensitivity.
Suspect #3 – Gluten Sensitivity comes in Many Forms
Similar to the above, gluten sensitivity can come in many forms – Celiac Disease, Non-Celiac Gluten Sensitivity or Wheat Allergy. While there are tests for celiac disease and wheat allergy, testing for non-celiac gluten sensitivity is not straightforward. This could be why many reported their eczema improving after cutting gluten yet they are not tested to be allergic to it.
There has been some (small scale, not conclusive) research suggesting that eczema sufferers tend to have gluten sensitivity which is why cutting gluten has worked for them.
Suspect #4 – Sugar Intolerance
For other eczema patients, cutting out sugar improves their eczema – a possible reason is that they have an intolerance to fructose or sucrose. This is due to the lack of digestive enzyme frutase and sucrase. However, tests for these are more expensive and being in many of processed foods and foods we eat, you may not think of testing for it.
Also cut the soda, read its harmful effects in this Soda and Child series.
Suspect #5 – Milk Intolerance
Similar to above, one could also be intolerant to milk from a lack of digestive enzyme lactase. It’s possible that the intolerance reaction gets triggered from different amounts and therefore, you may not know it’s from milk.
Read also alternative food sources from nutritionist Natalia Stasenko if your child is intolerant to milk.
Suspect #6 – Cutting out Inflammatory Foods
I’m personally very careful about NOT eating inflammatory foods and if your child with eczema is obese too, read tips from nutritionist Rania Batayneh on an anti-inflammatory diet.
The basic concept of inflammatory foods is that these foods promote the production of substances that put stress on our body, being increasingly recognized as the cause of many health conditions which are linked to prolonged inflammation (chronic inflammation). To understand this better, see interview with nutritionist Toby Amidor.
I’m not clear how inflammatory foods directly link with eczema but the general link is that eczema is skin inflammation (rash) and the overall reduction of inflammatory foods may have a greater impact on certain individuals than others (my own guess).
Suspect #7 – Eating Clean
This term ‘clean eating’ is quite ambiguous but generally taken to mean that we don’t eat processed foods, fried foods nor trans fat. There are also people that said once they cut out processed foods, cook and eat healthy, their eczema improved. I’m a big supporter of that, not so much for improving eczema but more for general health. In terms of research that supports doing so, there is a large scale association study that showed children who ate fast food more than 3 times/week are 30% more likely to have more severe allergic conditions. (side point – Prof Hywel Williams who led the study also wrote the foreword for my Living with Eczema book!)
Suspect #8 – Going Vegan
Some eczema sufferers choose to go vegan or cut down on meat. There is a basis for this as explained by dermatologist Dr Cheryl Lee in this post on Diet and Environment on Skin. Animal proteins and sugar are pro-inflammatory and give rise to excess free radicals that damage our body and our skin. My own guess is that some people get affected by animal protein more than others which is why going vegan works wonders for their skin!
Suspect #9 – Being Able to Take Action reduces Stress
This is my own guess – it is known that stress triggers eczema flare-ups (see dermatologist Dr Claudia Aguirre’s interview on Stressed Skin is Skin Deep) and most patients also feel helpless especially when there is no clear trigger or solution offered by their doctor. Being able to take proactive steps to eat healthy, cut sugar or figure out gluten-free recipes may reduce stress and inspire new interest in cooking. So the reduced stress possibly helps the eczema and for more on stress affecting acne, see dermatologist Dr Verallo-Rowell’s interview on Diet and Lifestyle.
Above is my thoughts on why eczema sufferers or parents of eczema children feel that changing diet ‘cured’ their eczema. Did diet change work for you? Share in the comments!
One reader, from Odylique Essential Care shared this post that they compiled from research papers and their infographic (Credit:www.odylique.com)
Last Saturday 28 March, the Eczema Support Group kickstart the year with a wet wrap session and I learnt something new every time!
The wet wrap demonstration was by Mölnlycke Health Care Limited, whose Tubifast product is used globally. A few tips about using wet wrap:
1. It can be dry or wet. Dry wrap is having a single layer of the bandage tubing over skin that has bee moisturized. Wet wrap is having an inner layer soaked in water, over moisturized skin and an outer layer over that inner layer. This applies for garments as well.
2. Different color-coded are of different sizes, the most common ones are green and blue sold in Guardian pharmacies, the smaller sized ones and garments are available in hospitals or the National Skin Centre.
3. Wet wrap can be hand washed, air dry (not in direct sun) and reused as long as it’s still elastic. You can refer to this post for more tips on wear and tear.
4. Size – Always cut a longer strip than the area to be wet wrapped, and there will be some fraying, fold the frayed ends in; and don’t keep trying to cut the frays away. Gloves are available, even for infants – they make look too small, but they are stretchable.
5. Materials – for garment, it is elastane, nylon and viscose and for wrap, viscose, elastane and polyamide. For those with latex allergy, no worries because no latex is used in the product nor the packaging.
6. Tie it up – Try tying knots to secure one part of the wrap to the next, perineal dressing, picture above. Basically cut a hole in one part of wrap, say body, and cut another on the hips, cut a thin strip and loop that strip through these two holes.
Thank you to all who attended and the National Skin Centre staff – subscribe at the blog top right corner to stay tuned for updates!
The past few weeks have really taken a toil on Kate. I totally totally know what she’s going through. For more cartoons on Kate and Mark, see here.

My kid has eczema and we haven’t figured out what is the trigger. I’ve been asking the doc about taking an allergy test but the doctor either say that my kid’s eczema is only at a certain area, so no testing is needed or say that it’s those common allergens that affect almost every child, so again no testing is needed. But there’s no CONCRETE EVIDENCE of WHAT’S TRIGGERING MY CHILD’S ECZEMA – why can’t the doc just give me the test?
Frustrated Mom
I totally understand, many moms feedback the same and many docs replied the same. The short reply is if taking an allergy test is on your mind 24/7, just demand it. If the dermatologist that you’re seeing refuses to prescribe one, go to another doctor. After all, eczema is a long-term situation that requires much working and communication with your doc; if you can’t even agree on something as basic as whether or not to allergy test, it’s unlikely that this is a doctor that you can work with.
On presenting both sides of the story:
From the parents’ view:
- You’re tearing your hair out figuring out the triggers, you need an allergy test to get some answers.
- You’re growing day by day fearful of applying corticosteroid cream on your child, figuring out the trigger means less flare-ups and less need for the steroid.
- You’re breastfeeding still and you seriously are going nuts on what you can or cannot eat.
From the doctors’ view:
- Your child’s eczema is localized, say on the face, thus likely due to saliva or food residue irritating the child’s skin.
- Allergy testing is unlikely to be accurate for a baby (less than 6 months) and therefore, testing and working on the inaccurate results may turn out to be even more confusing for the parents.
- It is true that most of the children are affected by the common allergens of cow’s milk, egg, soy, wheat, seafood, dust mite, pet dander and pollen. Younger children are more affected by food while older children are commonly affected by dust mite. It is therefore a waste of money to be testing for something when you’d already know the test results.
SkinishMom’s view:
- Go for allergy testing, even if it’s going to turn out results you’d expect (so you know for sure).
- Go for allergy testing at the clinic/hospital where you’d want to see the doctor, because the results have to be interpreted and collaborated, with future action plan for eczema care
- Don’t go for allergy testing online or some ‘innovative’ allergy tests – skin prick, blood IgE and skin patch are the standard tests
Do what you (as a mom/dad) think it’d give you peace,
SkinishMom

Toxic shock syndrome is rare but life threatening, caused by bacterial toxins from staphylococcus aureus. Toxic Shock Syndrome commonly affects teens and young adults, from age 15 to 35 and majority, female.
What Causes Toxic Shock Syndrome?
Toxic Shock Syndrome is due the bacterial infection via the skin, vagina or pharynx into the bloodstream. While it is not uncommon for Staph bacteria to colonize the skin, a cut, surgery or wound in some individuals may lead to the bacteria entering the blood without immunity to fight it. The conducive environment for the toxin is protein-rich and oxygen, which is what the use of tampons during menstruation provides. Tampons with higher absorbency (polyester, carboxymethylcellulose and polyacrylate) increases the risk of TSS. The toxins can cross the vaginal wall to the blood stream, possibly through tear when inserting the tampon.
Symptoms of Toxic Shock Syndrome
- Flu-like symptoms
- Confusion, dizziness due to low blood pressure
- Skin rash
- Swelling and redness in mucous membrane
- Shock
- Multi-organ failure
Diagnosis is made based on physical examination, blood or urine test or swaps from the cervix, vagina and throat.
Stages of Toxic Shock Syndrome
- High fever, sore throat, fatigue, muscle ache, nausea, fatigue, diarrhea, headache, dizziness (low blood pressure), confusion
- Reddish tongue, inflamed mucous membrane (eyes)
- Swelling of joints and eyelids
- Skin rash – generalized, flat and red (characterized by turning white when pressed)
- Shock occurs when the blood pressure cannot be maintained
- Skin rash disappears on recovery.
- Skin on palms of hands and soles of feet flake and peel off.
- Fingernails, toenails and hair may fall out.
Types of Toxic Shock Syndrome
- Toxic Shock Syndrome due to bacteria Staphylococcus aureus
- Streptococcal Toxic Shock Syndrome due to bacteria Streptococcus pyogenes
Treatment of Toxic Shock Syndrome
TSS is considered a medical emergency that required hospitalisation. An intravenous antibiotic will be prescribed to fight the bacteria infection, or medication to stabilize blood pressure and to prevent dehydration. Injections may also be given to suppress inflammation and increase body’s immunity. Also the cause of the bacterial infection will be removed, for instance, removal of the tampon or draining pus from the skin wound.
Complications of Toxic Shock Syndrome
If the internal organs are affected, it can lead to liver, kidney, heart failure, seizure and shock. Early detection of toxic shock syndrome has a much higher chance of recovery. The mortality rate is about 5-15% and rate of recurrence at 30-40%.
Toxic Shock Syndrome and Eczema
It is observed that patients recovering from TSS tend to develop chronic eczema. I couldn’t find literature on the likelihood of having TSS if one has eczema. I wonder if there’s increased risk since the skin of eczema patients tend to have staph bacteria colonization.
Prevention of Toxic Shock Syndrome
Certain precautions for menstruating female who uses tampon are to change the tampon every 4 to 8 hours and to use a low-absorbency tampon. Wash hands and keep skin cuts and wounds clean with frequent dressing change. TSS may recur, thus tampon should not be worn by those who had TSS before.
Anyone have experience with toxic shock syndrome? Do share, it will be useful to the rest of us and to be more aware of the risks.
For other life-threatening skin rash, see below:
Yes, some studies indicate evidence of behavioural disturbances for children with severe eczema from a young age (childhood anxiety, withdrawal, depression). Parents of eczema kids would know there’s likely psychological impact without reading research. Why?
- No Sleep, Brain can’t function – cranky.
- So much stress as an infant, something may just go wrong as the brain is wiring itself loads at that time. (If you’re a parent of a very young baby with eczema, you can visibly see the discomfort and agony caused by the itchy rash. Plain torture.)
- Being looked at with curious eyes. Being avoided. Being bullied.
- Whole family is stressed and short-fused. No one dare say living in such environment is conducive for health.
So how to reduce the chance of your kid going nuts?
The model answer is:
- Control the eczema, seek treatment.
- Recognize signs of depression.
- Seek a support group.
- Try relaxation techniques.
- Educate and raise awareness in your child’s school.
#SkinishMom answer is:
- Sleep whenever you can.
- Love yourself, love your spouse, love your child. The whole family united can take on challenges.
- Chill
- Indulge
- Positive mindset.
What’s your survival techniques?
#SkinishMom
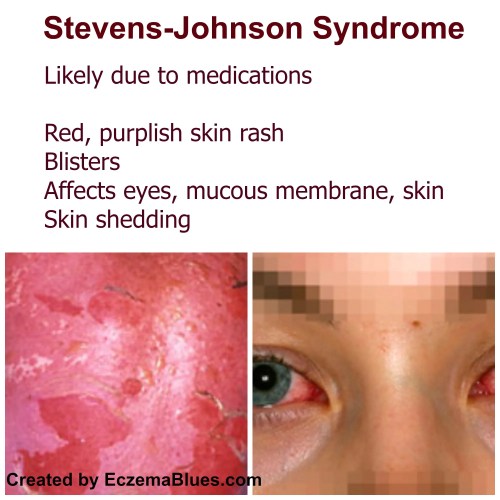
Stevens-Johnson Syndrome (SJS) is a rare, severe disorder that causes pain, red/purplish skin, blisters and shedding of skin. It can be drug-induced or due to infection. It is a medical emergency and takes from weeks to months to recover. It is more common in adults or older people and men who use more of the possible drugs that trigger the SJS.
What Causes Stevens-Johnson Syndrome?
Its cause is largely drug-induced (more than 70%) or due to infection. However, genetics, family history and weakened immune system are also risk factors.
From Mayo’s Clinic website:
- Anti-gout medications, such as allopurinol
- Pain relievers such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve)
- Medications to fight infection, such as penicillin
- Medications to treat seizures or mental illness (anticonvulsants and antipsychotics)
- Radiation therapy
The infectious causes listed by Medscape are:
Viral diseases:
- Herpes simplex virus
- AIDS
- Coxsackie viral infections
- Influenza
- Hepatitis
- Mumps
In children, Epstein-Barr virus, enteroviruses and upper respiratory tract infection.
Bacterial diseases:
- Group A beta-hemolytic streptococci
- Diphtheria
- Brucellosis
- Lymphogranuloma venereum
- Mycobacteria
- Mycoplasma pneumoniae
- Rickettsial infections
- Tularemia
- Typhoid
Symptoms of Stevens-Johnson Syndrome
- Flu-like symptoms
- Rash – Pain, Red, Purplish Skin
- Blisters
- Shedding Skin (Nikolsky’s sign)
- Eye-related – Painful red eye, purulent conjunctivitis, photophobia, blepharitis
Diagnosis is usually made via physical examination or skin biopsy.
Stages of Stevens-Johnson Syndrome
- Fever, sore throat or mouth sores
- Fatigue, cough, headache
- Swelling (face, tongue), Hives
- Rash – Pain, Red, Purplish Skin, Symmetric on face and torso
- Formation of blisters on skin and mucous membranes of mouth, nose, eyes, genitals
- Shedding of skin
Types of Stevens-Johnson Syndrome
The types are categorized by the extent of the body surface area (BSA) affected:
- Stevens-Johnson syndrome: Less than 10% BSA detached
- Toxic epidermal necrolysis: More than 30% of the BSA detached
Treatment of Stevens-Johnson Syndrome
Finding out the cause, in particular for drug-induced cases, is critical. Discontinue the drug. Treatment is to reduce pain, control itch, prevent dehydration, infection and inflammation. Oral corticosteroids and antibiotics may be prescribed. The patient is usually hospitalized.
Similar to Pemphigus Vulgaris, mouth/blister care is required.
Care of the Skin
Care of the skin includes application of lotions and wet dressings (wound care, wet compress). Particular to Stevens-Johnson Syndrome, eye care is also important to clean and prevent dry eyes.
Complications of Stevens-Johnson Syndrome
Complications include sepsis (blood infection), secondary skin infection (cellulitis), eye inflammation (tearing and scaring of cornea and even blindness) and permanent skin discoloration and damage (including nails).
Anyone have had SJS? Do share in the comments, thanks loads for spreading encouragement and experience.
I always wonder, does every mom really WILL HAVE ENOUGH MILK? For more cartoons on Kate and Mark, see here.

To #SkinishMom
Hey, this may seem like a minor, petty issue but color pencils, markers, crayons, poster colors are overflowing my kid’s play boxes and spilling to dining table tops. But I can’t stop buying them
- 1. They look so darn nice.
- 2. They are sometimes on sale.
- 3. Every new box of coloring keeps my kid occupied longer than an old box, which is VERY GOOD as it keeps the eczema scratching off!
But it’s increasingly becoming a point of contention – are we being materialistic? Is this encouraging hoarding? Is it wasteful? Is this not teaching my kid a sense of responsibility and inculcating frivolous-ism?
What do you think? Give me an honest answer.
Anonymous Mom
Wow, it’s like you read my mind. Have you been spying my daughter’s play boxes? I’ve 3 full boxes of coloring + stamping stuff. Honestly, yes, it’s wrong. No question.
Even more honestly, if you HAVE TO BUY them, buy them. In my usual investigative style, here’s the pros and cons to buying (and keep buying) that color pencil.
1. It makes you, as a mom who likes colors and doodling, happy.
2. It makes your kid happy.
3. It makes you feel like a good mom.
4. It keeps the eczema scratching off double the time with a new set of coloring.
5. It makes you be able to enjoy a restaurant meal with your spouse.
6. It is useful and spikes creativity.
The cons:
1. It is technically not a good use of money (to spend on stuff you already have loads of).
2. It makes your kid think he/she only uses new stuff.
3. It may make your spouse upset if both don’t see the pros.
4. It clutters your home and creates work when you clean up.
5. The coloring markers may dry up if not used, rendering something useful, useless.
So – 6 pros, 5 cons, go for it.
Checking out the latest cool stationery this weekend,
#SkinishMom

Hi to Singaporean readers!
On 28 March, Saturday, the Eczema Support Group under the National Skin Centre has organized a wet wrap demonstration and presentation, in collaboration with Tubifast. The session will have
- Presentation by Mölnlycke Health Care, the company with Tubifast wet wrap (read here to understand more on wet wrap)
- Wet wrap demonstration – How to do a double-layer wrap, moist inner layer with a dry outer layer
- Wet wrap sizes and techniques – It can get quite difficult to wrap parts with bends or that slip off + how to wet wrap for younger kids
A study had been released on the efficacy of wet wrap, citing a 71% reduction in symptoms out of the 72 children who took part in the study. Healthy skin is maintained one month after returning home with reduced reliance on medication. So come and learn this technique to add to your ‘arsenal’ of skincare for dry, eczema skin!
28 March 2015 (Saturday) – Venue, National Skin Centre Singapore Room 401, 9.45 am to 11.15 am
The program:
1. 9.45 am to 10.00 am Breakfast and Kids have balloon sculpture and jigsaw puzzles to keep them occupied
2. 10.00 to 11.00 am Tubifast demonstration and presentation
3. 11.00 to 11.15 am Q&A time
Note:No doctor will be present but a senior dermatologist, Sister Wong who is an esteemed guest speaker for our group will be attending. No selling anything or pretending to be a parent of eczema child and the session is for parents with eczema kids. Information on my blog is not pre-approved by NSC.
4. YOU MUST RSVP – It will then be possible for us to prepare breakfast and for the Tubifast team to prepare the relevant product. If you’re coming, please email me ([email protected]) your name, mobile and email, number of adults & kids (and age, so the right size wrap can be prepared for presentation) coming.
One last thing, the session would be ending on-time, so please don’t come late and expect it to drag, it won’t – simply cos I have to run! Look forward to seeing you! Mei
Pemphigus Vulgaris (PV) is a rare, auto-immune disease that mistakes skin cells and mucous membranes as foreign matters and attacks them. This results in blisters and sores of the skin and the mucous membranes. It is more common in middle-aged and older people. PV is not infectious.
What Causes Pemphigus Vulgaris?
Pemphigus vulgaris is caused by an increase in the desmoglein antibodies where these antibodies incorrectly binds to protein desmoglein 3, which is found in desmosomes in the keratinocytes near the bottom of the epidermis. It then results in a separation of the skin layer and formation of blisters. The triggers of this faulty immune systems are not fully known though genetics play a part.
Types of Pemphigus Vulgaris
Mucosal PV: Only the mucous membranes are affected, but not the skin. This may include the mucous membranes lining the mouth, nose, throat and genitals.
Mucocutaneous PV: Both the mucous membranes and skin are affected.
Symptoms of Pemphigus Vulgaris
- Fever, Chills
- Muscle aches
- Rash, first appearing in mouth and then to rest of the skin
- Blisters
- Raw, moist, tender skin
- Peeling Skin
- Fluid loss
- Pain
Diagnosis is usually made by a skin specialist because it is uncommon, thus not often seen by general practitioners. Physical examination and lesion biopsy (including immunofluorescence to assess level of antibodies) are used to diagnose PV. Early treatment helps to prevent PV from being widespread.
Stages of Pemphigus Vulgaris
- Formation of blisters and sores around the mouth
- Bursting of mouth blisters, similar to ulcers
- More widespread blisters at other parts of skin with oozing, crusting and peeling of skin.
- Separation of outer layer skin with gentle touch (“Nikolsky’s sign”)
- Recovery of raw skin (6 to 8 weeks)
Treatment of Pemphigus Vulgaris
There is no treatment that specifically cures PV but instead treatment is to reduce blistering and limit flare-up. This is often via immunosuppressant therapy. Oral corticosteroids and immunosuppressive drugs may be prescribed. In more severe cases, it can be via intravenous methylprednisolone and cyclophosphamide (Pulsed therapy) which can last from 6 months to a year. Dosages are typically higher at the start of treatment and gradually reduces when the condition is stable (without flare-up).
For severe cases, the patient will be hospitalized in the burn unit as the skin requires similar care to burns. Apart from immunosuppressant therapy, treatment also encompasses (i) pain relief, (ii) anesthetic lozenges to reduce mouth ulcer pain, (IiI) prevention of dehydration through intravenous drip, (Iv) medication to prevent bacterial or fungal infection
Care of the Skin
Care of the skin includes application of lotions and wet dressings (wound care, wet compress). Also minimize contact sports to avoid skin trauma.
Mouth Blisters and Care
If blisters occur in the voice box (larynx), the voice will be hoarse. If the blisters occur in the gullet, swallowing is painful. Where mouth blisters make it difficult to eat, supplements may be prescribed. Steroid, antiseptic or anesthetic mouth wash may also be prescribed for the mouth blisters. Avoid foods that may irritate the inside of mouth such as spicy, acidic or hard foods.
Pemphigus Vulgaris and Eczema
PV is sometimes diagnosed late as mistaken for dyshidrotic eczema or pompholyx which also has blisters. However, dyshidrotic eczema is not life threatening and believed to be due to stress or allergies.
Complications of Pemphigus Vulgaris
It is a difficult condition to treat as it is an autoimmune disease that has no cure. The mortality rate is 10%. There can also be complications associated with long-term use of oral corticosteroids and immunosuppressants. Other complications are secondary skin infection, dehydration and sepsis (bloodstream infection).
Anyone have had PV? Do share in the comments, thanks loads for spreading encouragement and experience!
I totally empathize with this one.
Don’t say there isn’t enough place to store your breast milk in front of Mommy Kate. For more cartoons on Kate and Mark, see here.
 That’s difficult. Hypocritical to answer if I have not been through the darkest hour. So, I asked MarcieMom:
That’s difficult. Hypocritical to answer if I have not been through the darkest hour. So, I asked MarcieMom:
MarcieMom: There was one night I remembered – one night after many months of waking up in the middle of the night for 2-4 hours to wipe my baby’s skin with chlorhexidine, moisturize again, change new PJs, feed a snack and prep for bedtime all over again. On this one night, the day had been very bad. I had to hold my baby’s hands almost throughout the day, the stress of not taking a second off and feeling alone.
Feeling that God had turned his back on my baby.
Wondering why God had intended for my baby to suffer.
There was no answer.
Yet, in some way, God answered. Within about 2 months, Marcie was tested not allergic to anything and responded well to treatment.
Within 6 months, I started EczemaBlues to help other parents.
Where is God in my darkest hour? He was with me – I did not feel it then but my spouse stood by me and we pulled through.
Bible verses for you to hang onto during dark times:
John 14:1 – Let not your hearts be troubled. Believe in God; believe also in me.
Proverbs 3:5-6 – Trust in the LORD with all your heart, and do not lean on your own understanding. In all your ways acknowledge him, and he will make straight your paths.
Matthew 11:28-30 – “Come to me, all who labor and are heavy laden, and I will give you rest. Take my yoke upon you, and learn from me, for I am gentle and lowly in heart, and you will find rest for your souls. For my yoke is easy, and my burden is light.”
2 Corinthians 4:16-18 – So we do not lose heart. Though our outer self is wasting away, our inner self is being renewed day by day. For this light momentary affliction is preparing for us an eternal weight of glory beyond all comparison, as we look not to the things that are seen but to the things that are unseen. For the things that are seen are transient, but the things that are unseen are eternal.
Staphylococcal scalded skin syndrome (SSSS) is one skin rash that affects children (newborn to 5 years old), caused by infection from certain strains of Staphylococcus aureus bacteria. The bacteria produces toxins (epidermolytic toxins A and B) that bind to a molecule within the part of skin cell (demosomes) that adhere skin cells together. The damaged desmosome cannot continue to adhere skin cells and the skin break up, leading to fluid filling in the spaces (blisters) and peeling skin.
What Causes Staphylococcal Scalded Skin Syndrome?
Staphylococcal scalded skin syndrome is caused by certain toxic strains (exotoxin of group II, phage type 71) of the staphylococcus bacteria found on skin. However, when there is broken skin from scratching, cut, a minor infection that can escalate to SSSS in children and in people with weakened immune system or renal insufficiency.
Symptoms of Staphylococcal Scalded Skin Syndrome
- Fever
- Chills
- Lethargy
- Skin redness (Erythema)
- Blisters
- Raw, moist, tender skin
- Peeling Skin
- Fluid loss
- Physical examination is often sufficient to diagnose SSSS. Where unsure, other tests like skin biopsy, blood tests may be ordered.
Stages of Staphylococcal Scalded Skin Syndrome
Begins with signs of infection like fever, chills and irritability
Followed by skin redness and formation of lesions – for infants, lesions often start at diaper area or at umbilical cord (triggered by other conditions such as purulent conjunctivitis, nasopharyngeal infection or an infected umbilicus). For older children, usually the flexural areas and skin folds like the face, mouth/nose, neck, groin and armpit (triggered by impetigo or infected eczema or wound infection).
Skin wrinkles and Formation of blisters – Irregular, large and loose blisters
Rupturing of blisters
Formation of yellow crust, followed by drying and cracking
Peeling of outer layer skin (Exfoliation) – Revealing red, raw and wet skin. The outer skin falls off with gentle pressure, known as the Nikolsky’s sign.
Recovery of raw skin (takes from 5 to 10 days)
Treatment of Staphylococcal Scalded Skin Syndrome
Hospitalization is often required, at the burn unit of the hospital as the risk of complication is similar to burns. Treatment options include
- antibiotics to treat the staph bacteria infection,
- drip to prevent dehydration and
- care of the skin.
With SSSS, the child will feel pain at the skin and experience fluid and heat loss via exposed skin. Therefore, treatment will include caring for the child in a warm environment with minimal clothing. Pain control such as analgesia and paracetamol may be given to the child. The child should drink extra fluids to replenish the excess moisture loss from skin and prevent dehydration (check weight and urine for signs of dehydration).
Care of the Skin
Given the fragile skin, care must be taken when handling the skin to reduce trauma, such as when administering intravenous drips, creams and using non-adherent dressing to prevent further tearing of the skin. Moisturizer is applied to reduce fluid loss and soothe the skin until full recovering with smooth skin.
Staphylococcal Scalded Skin Syndrome and Eczema
Severe eczema presents higher risk due to broken skin (with scratching) and higher chance of staph bacteria colonization.
Complications of Staphylococcal Scalded Skin Syndrome
For children who are treated promptly, there is a high chance of recovery without scarring (mortality rate below 5%). In adults, it can be life threatening.
Other possible complications are cellulitis (deeper skin infection), sepsis (bloodstream infection) and pneumonia, though not common.
Prevention of Staphylococcal Scalded Skin Syndrome
Prevention of outbreaks in neonatal and nursery day cares are critical – adults who carry the bacteria (5% of adults) can spread to infants who may develop SSSS due to weaker immunity. Isolating the infected healthcare worker, hand washing and alcohol hand rubs should be practiced in the ward. Towels should not be shared.
If you have experienced SSSS, do share in the comments, thanks!