Do you feel like you have tried everything to help your child manage his eczema but your efforts seem to be futile? Turn your attention to the skin microbiome, in particular, staphylococcus aureus (staph bacteria).
This is a 2-week series focused on Gladskin’s targeted approach in improving eczema skin, through maintaining a healthy skin microbiome. I’m honored to have the President of Gladskin USA, Skyler Stein, to help in this series. Read his bio here.

We were alerted early that staph bacteria is a harmful bacterium that colonizes eczema skin, that makes the eczema treatment less effective. Since my daughter was seven months old, she started chlorhexidine wipes and swimming. Now at ten years old, she is still using an anti-microbial cleanser.
An Enemy that is Hidden in Plain Sight & Cannot be Killed
Yet, when my daughter recently had skin swap tests on an infected persistent eczema rash, she was tested positive for staph bacteria. This was even with the thrice weekly anti-microbial skin wash. I was shocked that with all that regular anti-microbial cleansing (which I already feared may be a bit too much), the staph bacteria were still proliferating. It almost felt like we were battling with a hidden in plain sight enemy that cannot be killed!
Gladskin’s Targeted Approach – Taking out the Bad Bacteria, without taking down the Good Bacteria
The prevalence and proliferation of staph bacteria on eczema skin is a tricky situation. You have to remove the staph bacteria but doing so through bleach bath, swimming (chlorine) or anti-microbial wash would mean killing the good bacteria on the skin as well. And very often, these methods may be drying for the skin.
Gladskin has developed a patented smart protein Micreobalance which rebalances the skin microbiome in a very targeted way. while protecting the good bacteria on the skin.

A Step Back: What is the Big Deal with Skin Bacteria?
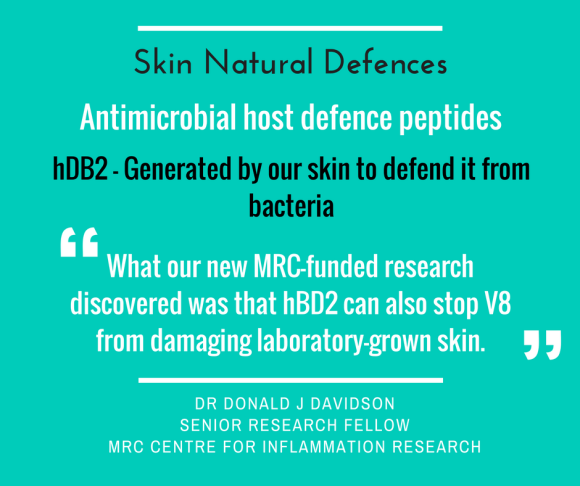
Our skin is home to millions of microbes, and there are both beneficial and harmful bacteria. The harmful bacteria causes inflammation and infection – of concern for eczema patients is staph bacteria, which worsens eczema. For instance, staph bacteria1:
- Reduces the biodiversity of skin microbiome, which would also reduce beneficial bacteria and upset the skin’s healthy microbiome
- Produces byproducts that causes inflammation
- Severity of eczema correlates with increased staph bacteria
MarcieMom: I really like the targeted approach for Gladskin product because it makes perfect sense! The main benefit versus anti-microbial products would be not killing the beneficial bacteria. Can you give us an idea of how long it takes for the good bacteria to ‘grow’ back on our skin?
Skyler Stein: Yes, the targeted approach with Gladskin is what makes it truly a new category of treatment for people with eczema.
The answer to this question about how long it takes for good bacteria to grow is complicated as there are thousands of different types of “good” bacteria, and different types of bacteria take different amounts of time to grow. The most important thing to realize is that if you kill the good bacteria, it creates an environment more favorable for the bad bacteria to thrive – so it’s really important to maintain a healthy skin microbiome for long term skin health.
MarcieMom: I’m thinking about the ‘practical’ logic behind using Gladskin. For instance, if I were to use an anti-microbial wash daily on my child to kill staph bacteria, would it be difficult for the good bacteria to build up on her skin?
Skyler Stein: Yes, if you use a broad spectrum antimicrobial on the skin, it will kill both the good and bad bacteria. In a healthy rainforest with lots of biodiversity, the ‘good’ plants naturally keep invasive weeds from growing out of control. If you burn down the rainforest, killing all the biodiversity, it is much more likely for invasive weeds to grow out of control. It works the same way on your skin, if you kill the good bacteria, it creates an environment that allows the bad bacteria to take over!
MarcieMom: Can you explain how daily washing of beneficial bacteria may hurt the child’s skin?
Skyler Stein: The beneficial bacteria on the skin are like little chemical factories that produce lipids, vitamins, nutrients, etc. that are essential for healthy skin, AND they keep the bad bacteria in check. If you kill the good bacteria, the skin will miss out on the essential ingredients produced by those bacteria that are needed for healthy skin, and creates an opportunity for the bad bacteria to grow out of control.
If you kill the good bacteria, the skin will miss out on the essential ingredients produced by those bacteria that are needed for healthy skin, and creates an opportunity for the bad bacteria to grow out of control.
Spotlight on the Active Ingredient – Micreobalance™
MarcieMom: I read on your FAQ page that the ideal temperature for storage is below 75 ºF. Is this going to affect whether you sell the products in tropical countries, or affect storage during the hot summer months? Would you discourage parents from bringing your cream out to the park on a hot day?
Skyler Stein: Gladskin can withstand temperatures of over 100ºF for a week, and 3 months at room temperature. If you plan to keep Gladskin longer than 3 months we recommend storing it in the refrigerator. It’s safe to take with you to the park on a hot summer day, but we don’t recommend keeping it in a hot car for months.
Thank you Skyler for giving us a broad understanding of the beneficial and harmful bacteria on eczema skin and why it’s so important to keep a healthy balance of bacteria for healthy skin. You can learn more about Gladskin’s science and read reviews from current Gladskin users at www.gladskin.com. Continue to next week’s interview with Skyler.
Sponsored Post by Gladskin
References:
- The bacterial culprit that drives atopic dermatitis. NationalEczema.org